Diagnosis of Alzheimer’s Disease
PET scans of the brain in Alzheimer’s disease show a decline in activity in the temporal lobes.
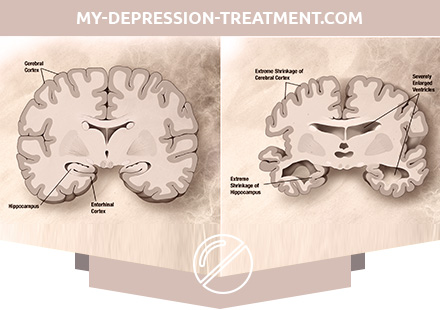
The clinical diagnosis of Alzheimer’s disease is usually based on the patient’s history (a history of life), the history of his relatives and clinical observations (hereditary history), taking into account the characteristic neurological and neuropsychological signs and excluded alternative diagnoses. In order to distinguish the disease from other pathologies and varieties of dementia, complex medical imaging techniques such as computed tomography, magnetic resonance imaging, photon emission computed tomography or positron emission tomography can be used. [90] For a more accurate assessment of the state, intellectual functions are tested, including memory. Medical organizations develop diagnostic criteria in order to facilitate the diagnosis of the practitioner and standardize the process of diagnosis. Sometimes the diagnosis is confirmed or established posthumously by histological analysis of brain tissue.
Diagnostic criteria for Alzheimer’s disease
The National Institute of Neurological and Communicative Disorders and Stroke (NINDS) and the Alzheimer’s Disease Association formed the most frequently used set of criteria for diagnosing Alzheimer’s disease. According to the criteria, for making a clinical diagnosis of possible Alzheimer’s disease, it is required to confirm the presence of cognitive impairment and presumptive dementia syndrome during neuropsychological testing. For final confirmation of the diagnosis, a histopathological analysis of brain tissues is necessary, and during the verification of in vivo diagnoses by criteria with posthumous analysis, good statistical reliability and verifiability were noted. Most often, disorders in Alzheimer’s disease affect eight domains: memory, language skills, ability to perceive the environment, constructive abilities, orientation in the space of time of his own personality, problem solving skills, functioning, self-sustainment.
These domains are equivalent to the NINCDS-ADRDA criteria listed in the DSM-IV-TR.
Diagnostic tools
In the diagnosis of Alzheimer’s disease can help neuropsychological screening testing, in which patients copy figures, memorize words, read, perform arithmetic operations.
PET scan: In Alzheimer’s disease, the Pittsburgh composition B introduced into the body accumulates in the brain, becoming attached to beta-amyloid deposits (left). On the right is an older person’s brain with no signs of Alzheimer’s disease.
Neuropsychological tests, such as MMSE, are widely used to assess cognitive impairment that must be present in a disease. To obtain reliable results, more extensive test sets are required, especially in the early stages of the disease. At the onset of the disease, a neurological examination usually shows nothing unusual, with the exception of obvious cognitive abnormalities that may resemble ordinary dementia. Therefore, for the differential diagnosis of Alzheimer’s disease and other diseases, an extended neurological examination is important. Interviews with family members are also used in assessing the course of the disease, since relatives can provide important information about the level of a person’s daily activity and about a gradual decrease in his mental abilities. Since the patient himself usually does not notice the violations, the point of view of the people caring for him is especially important. At the same time, in many cases, the early symptoms of dementia go unnoticed in the family and the doctor receives inaccurate information from relatives. Additional tests enrich the picture with information about some aspects of the disease or allow to exclude other diagnoses. A blood test can reveal alternative causes of dementia, which occasionally even respond to therapy that reverses the symptoms. Psychological tests are also used to detect depression, which can either accompany Alzheimer’s disease or cause cognitive decline.
Equipment SPECT- and PET-visualization with its availability can be used to confirm the diagnosis together with other assessment methods, including the analysis of mental status. In people who already suffer from dementia, SPECT, according to some sources, makes it possible to more effectively differentiate Alzheimer’s disease from other causes, as compared with standard testing and anamnesis. The ability to observe beta-amyloid deposits in the brain of living people was created by the creation of the Pittsburgh compound B (PiB) at Pittsburgh University, which binds to amyloid deposits when introduced into the body. The short-lived radioactive isotope carbon-11 in the compound allows you to determine the distribution of this substance in the body and obtain a picture of amyloid deposits in the patient’s brain using a PET scanner. It was also shown that the content of beta-amyloid or tau protein in the cerebrospinal fluid can be an objective marker of the disease. These two new methods led to proposals for the development of new diagnostic criteria.
Alzheimer’s Disease Treatment
Alzheimer’s disease cannot be cured; available therapies can have a small effect on the symptoms, but are inherently palliative. From the whole complex of measures, pharmacological, psychosocial and patient care measures can be distinguished.
Pharmacotherapy
Regulatory agencies such as the FDA and EMEA have now approved four drugs for the treatment of cognitive impairment in Alzheimer’s disease — three cholinesterase inhibitors and memantine, an NMDA antagonist. At the same time there are no such drugs, among the actions of which it would be indicated to slow down or stop the development of Alzheimer’s disease.
A known sign of Alzheimer’s disease is a decrease in the activity of cholinergic neurons. Cholinesterase inhibitors decrease the rate of acetylcholine (ACh) destruction, increasing its concentration in the brain and compensating for the loss of ACh caused by the loss of cholinergic neurons. As of 2008, doctors used such ACh-inhibitors as donepezil, galantamine, and rivastigmine (in the form of tablets and patches). There is evidence of the effectiveness of these drugs in the initial and moderate stages, as well as some reasons for their use at a later stage. Only donepezil is approved for use in severe dementia. The use of these drugs for mild cognitive impairment has not delayed the onset of Alzheimer’s disease. Among the side effects of drugs, the most common are nausea and vomiting associated with an excess of cholinergic activity, they occur in 10-10% of patients and may be mild or moderately expressed. Less common muscle spasms, bradycardia, loss of appetite, weight loss, increase in acidity of gastric juice.
The excitatory neurotransmitter glutamate plays an important role in the nervous system, but its excess leads to excessive activation of glutamate receptors and can cause cell death. This process, called excitotoxicity, is noted not only in Alzheimer’s disease, but also in other conditions, such as Parkinson’s disease and multiple sclerosis. A drug called memantine, originally used in the treatment of influenza, inhibits the activation of glutamate NMDA receptors. The moderate efficacy of memantine in moderate and severe Alzheimer’s disease has been shown, but it is unknown how it acts at an early stage. Rarely observed mild side effects, among them – hallucinations, confusion, dizziness, headache and fatigue. In combination with donepezil, memantine demonstrates a “statistically significant, but clinically barely noticeable efficacy” in acting on cognitive performance.
In patients whose behavior is a problem, antipsychotics can moderately reduce aggression and affect psychosis. At the same time, these drugs cause serious side effects, in particular, cerebrovascular complications, motor impairment and reduced cognitive abilities, which precludes their daily use. With the prolonged prescription of antipsychotics for Alzheimer’s disease, increased mortality is noted.
Psychosocial intervention
“Sensory Integrative Therapy”: a special sensory room (eng. Snoezelen) is used for emotionally-oriented care for people suffering from dementia.
Psychosocial intervention complements the pharmacological and can be divided into the following approaches:
- behavioral;
- emotional;
- cognitive;
- stimulatory-oriented.
The effectiveness of the intervention has not yet been covered in the scientific literature; moreover, the approach itself does not extend to Alzheimer’s disease, but to dementia as a whole.
Behavioral intervention is aimed at identifying the prerequisites and consequences of problem behavior and working to correct them. When using this approach, there is no improvement in the overall level of functioning, but it is possible to alleviate some of the individual problems, such as incontinence. Regarding the effect of the techniques of this direction on other behavioral deviations, such as wandering, there is not enough qualitative data accumulated.
Interventions that affect the emotional sphere include memory therapy (reminiscence therapy, RT), validation therapy, supportive psychotherapy, sensory integration (“snoozelen”), and “simulated presence therapy” (SPT). Supportive psychotherapy has almost not been studied by scientific methods, but some clinical workers believe that it provides benefits when trying to help patients with ill health adapt to the disease. In memory therapy (RT), patients discuss their experiences face to face with the therapist or in a group, often using photographs, household items, old music and archival audio recordings, and other familiar objects from the past. Although the number of qualitative studies on the effectiveness of RT is small, a positive effect of this method on the patient’s thinking and attitude is possible. Presence simulation based on attachment theories involves playing back audio recordings with the voices of the next of kin. According to preliminary data, patients undergoing a course of SPT, decreases the level of anxiety, the behavior becomes calmer. Validation therapy is based on the recognition of the reality and personal truth of the experiences of another person, and during sensory integration sessions the patient performs exercises designed to stimulate the senses. There is little data to support these two methods.
Orientation in reality, cognitive retraining and other cognitive-oriented therapies are used to reduce the cognitive deficit. Orientation in reality consists in presenting information about the time, location and personality of the patient in order to facilitate their awareness of the situation and their own place in it. In turn, cognitive retraining is carried out to improve the impaired abilities of the patient, who is given tasks that require mental exertion. Some improvement in cognitive abilities was noted with the use of both the first and second methods, but in some studies this effect disappeared with time and negative manifestations were noted, for example, patient frustration.
Stimulating therapies include art therapy, music therapy, as well as types of therapy in which patients communicate with animals, exercise, and any other restorative activity. Stimulation, according to research, has a moderate effect on behavior and mood, and even less on the level of functioning. Be that as it may, such therapy is carried out mainly to improve the daily lives of patients.
Prevention of Alzheimer’s Disease
Intellectual activity, including the fascination with the game of chess, and regular communication correlate with a reduced risk of developing Alzheimer’s disease, according to epidemiological studies, however, a causal link has not yet been proven.
International studies designed to assess how this or that measure can slow down or prevent the onset of the disease often give conflicting results. To date, there is no solid evidence of the preventive effect of any of the factors considered. At the same time, epidemiological studies suggest that some corrective factors — diet, cardiovascular risk, medication, mental activity, and others — are associated with the likelihood of developing the disease. However, real evidence of their ability to prevent illness can be obtained only in the course of additional study, which will include clinical studies.
Ingredients of the Mediterranean diet, including fruits and vegetables, bread, wheat and other cereals, olive oil, fish and red wine, may, individually or together, reduce the risk and alleviate the course of Alzheimer’s disease. Acceptance of some vitamins, including B12, B3, C and folic acid, has been associated with a reduced risk of developing the disease in some studies, but other studies indicate the absence of a significant effect on the onset and course of the disease and the likelihood of side effects. Curcumin, which is contained in a common spice, when tested in mice showed some ability to prevent certain pathological changes in the brain.
Risk factors for cardiovascular diseases, such as high cholesterol and hypertension, diabetes, smoking, are associated with an increased risk and more severe course of Alzheimer’s disease, but cholesterol-lowering drugs (statins) have not been effective in preventing it or improving the condition of patients. The long-term use of nonsteroidal anti-inflammatory drugs is associated with a reduced likelihood of developing the disease in some people. Other medications, such as hormone replacement therapy in women, are no longer considered effective in preventing dementia. A systematic review of ginkgo biloba, conducted in 2007, indicates the inconsistent and inconclusive nature of the evidence on the effects of the drug on cognitive impairment, and another study suggests that there is no effect on the incidence.
Intellectual exercises, such as reading, board games, solving crossword puzzles, playing musical instruments, regular communication, may possibly slow the onset of the disease or mitigate its development. Bilingual knowledge is associated with a later onset of Alzheimer’s disease.
Some studies suggest an increased risk of Alzheimer’s disease in those people whose work involves exposure to magnetic fields, ingestion of metals, especially aluminum, or the use of solvents. Some of these publications have been criticized for their poor quality of work; moreover, other studies have not found a link between environmental factors and the development of Alzheimer’s disease.